Retropubic Suspension Surgery
Make an Appointment
Our team is here to help you make an appointment with the specialists that you need.
Retropubic Suspension Surgery
Surgery Overview
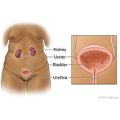
Retropubic suspension surgery is used to treat urinary incontinence. It lifts the sagging bladder neck and urethra that have dropped abnormally low in the pelvic area. The doctor makes a cut (incision) in the belly wall to access the bladder and urethra. This surgery can be done by making one big incision (open surgery) or several small incisions (laparoscopic surgery).
Burch colposuspension is the most common procedure used for retropubic suspension. The vaginal wall is attached to a ligament (Cooper's ligament) next to the pubic bone.
What To Expect
To allow the urinary tract to heal, a temporary catheter may be placed into the bladder through the urethra (or belly wall) to allow urine to drain.
You will likely go home 1 to 2 days after the surgery if there have been no complications. How long it takes to recover depends on which type of surgery you had.
If you had laparoscopic surgery, you will probably be able to go back to work in 1 to 2 weeks. If you had open surgery, it may take longer, about 2 to 4 weeks. For either surgery, you will need at least 6 weeks to fully recover before returning to all normal activities. You must avoid heavy lifting and strenuous activities during this time. These might put extra pressure on your bladder.
How much pain you have after surgery depends on the exact nature of your procedure, your health at the time of surgery, and your own response to pain. You will probably feel some pain at the incision site and may feel some cramping in your belly. Your doctor will prescribe medicine to relieve your discomfort during the first few days after surgery. Be sure to call your doctor if you can't get relief from pain.
Why It Is Done
Retropubic suspension is used to correct stress incontinence that is caused by sagging of the urethra and/or bladder neck.
How Well It Works
Retropubic suspension works to relieve stress incontinence. Most women have fewer symptoms of stress incontinence after this surgery.
For stress incontinence, doctors have been doing Burch colposuspension surgeries longer than sling surgeries. Many studies have been done on the Burch colposuspension surgery. About 9 out of 10 women are cured ("dry") during the year after surgery. After 5 years, about 7 out of 10 women are still "dry."footnote 1
Risks
Problems from retropubic surgery may include:
- Trouble urinating after surgery.
- New symptoms of urgency or urge incontinence.
- Internal bleeding.
- Infection at the incision site.
- Injury to an organ (such as the bladder, urethra, or ureters).
- Pelvic organ prolapse (usually, enterocele).
All surgeries that use general anesthesia have a small risk of death or complications. All surgeries carry some risk of infection.
Credits
Current as of: April 30, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: April 30, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024-2025 Ignite Healthwise, LLC.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.